What is Endometriosis?
Endometriosis is a chronic condition where tissue similar to the lining of the uterus (endometrium) grows outside the uterus. This abnormal tissue can be found on the ovaries, fallopian tubes, outer surface of the uterus, and other pelvic organs. Unlike the normal endometrial lining, which sheds during menstruation, this tissue has no way to exit the body, leading to inflammation, pain, and scarring.
Women with endometriosis often experience severe menstrual cramps, pelvic pain, and sometimes difficulty in conceiving. Since the condition can impact fertility, seeking timely medical intervention is crucial. For those facing challenges in achieving pregnancy, consulting the Best IVF Center in Vizag can provide effective treatment options and improve the chances of conception.
Stages of Endometriosis
Endometriosis is classified into four stages based on the severity, location, and extent of tissue growth. The American Society for Reproductive Medicine (ASRM) defines these stages as:
Stage 1: Minimal
• Description: Small patches, surface lesions, or mild inflammation are found on the ovaries or pelvic lining.
• Impact on Fertility: Minimal effect on fertility, but inflammation may disrupt the normal reproductive process.
Stage 2: Mild
• Description: More extensive tissue growth, with shallow implants on the pelvic lining and ovaries. Small adhesions may form.
• Impact on Fertility: Mild scarring may cause slight hindrance to egg movement and fertilization, potentially affecting conception.
Stage 3: Moderate
• Description: Deep implants, extensive scar tissue, and adhesions around the ovaries and fallopian tubes. Cysts, known as endometriomas, may form on the ovaries.
• Impact on Fertility: The chances of natural conception are reduced due to the formation of cysts and blockage of fallopian tubes.
Stage 4: Severe
• Description: Widespread tissue growth, deep implants, and extensive adhesions involving multiple pelvic organs. Large endometriomas may be present.
• Impact on Fertility: High risk of infertility due to distorted pelvic anatomy, blocked fallopian tubes, and compromised ovarian function.
Impact of Each Stage on Fertility
Endometriosis is categorized into four stages based on the severity, extent, and location of the abnormal tissue growth. Each stage affects fertility differently, with higher stages posing greater challenges to natural conception.
Stage 1: Minimal
• Description: Small lesions and minimal scar tissue are present on the pelvic lining or ovaries.
• Impact on Fertility:
◦ Fertility is generally not significantly impacted at this stage.
◦ Mild inflammation may interfere with sperm-egg interaction, but most women can conceive naturally.
◦ However, untreated minimal endometriosis can progress to more advanced stages, increasing the risk of infertility.
Stage 2: Mild
• Description: More pronounced tissue growth with shallow implants and mild adhesions.
• Impact on Fertility:
◦ Mild adhesions may affect the movement of the egg through the fallopian tubes.
◦ Sperm motility and fertilization may be slightly compromised due to inflammation.
◦ While natural conception is still possible, the chances may be reduced compared to women without endometriosis.
Stage 3: Moderate
• Description: Deep implants with scar tissue and adhesions, often accompanied by ovarian cysts called endometriomas.
• Impact on Fertility:
◦ The formation of adhesions and cysts may obstruct the fallopian tubes, preventing the egg and sperm from meeting.
◦ Ovarian function may be compromised, leading to reduced egg quality.
◦ Women in this stage often experience difficulties in conceiving naturally and may require assisted reproductive techniques (ART) like IUI or IVF.
Stage 4: Severe
• Description: Extensive lesions, deep implants, and large adhesions involving multiple pelvic organs. Large endometriomas may be present on the ovaries.
• Impact on Fertility:
◦ Severe distortion of pelvic anatomy, with blocked fallopian tubes and compromised ovarian function.
◦ High risk of infertility due to extensive scarring and poor egg quality.
◦ Women with severe endometriosis often require advanced fertility treatments, such as IVF, to achieve pregnancy.
Common Symptoms and Diagnosis
Endometriosis presents a wide range of symptoms, which can vary from mild to severe depending on the stage. Recognizing these symptoms early can help ensure timely diagnosis and treatment.
Common Symptoms of Endometriosis
• Pelvic Pain: Persistent or cyclical pelvic pain, often worse during menstruation.
• Painful Periods (Dysmenorrhea): Severe cramping and lower abdominal pain that may last beyond the menstrual period.
• Pain During Intercourse: Pain or discomfort during or after sexual intercourse, which may worsen over time.
• Heavy or Irregular Menstrual Bleeding: Prolonged periods or spotting between cycles.
• Painful Bowel Movements or Urination: Discomfort, particularly during menstruation.
• Chronic Fatigue and Bloating: Persistent exhaustion and a feeling of fullness.
• Infertility: Difficulty conceiving despite regular, unprotected intercourse.
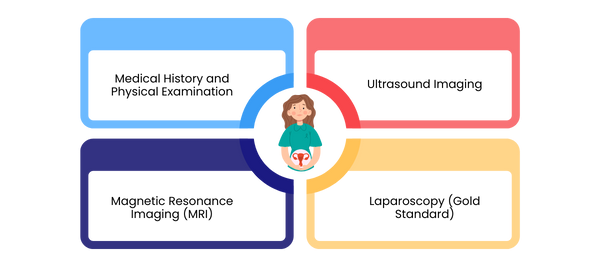
Diagnosis of Endometriosis
Diagnosing endometriosis can be challenging, as symptoms often overlap with other reproductive or gastrointestinal conditions. Common diagnostic methods include:
1. Medical History and Physical Examination:
◦ Detailed evaluation of menstrual history and pelvic pain.
◦ Pelvic examination to identify abnormalities or tenderness.
2. Ultrasound Imaging:
◦ Transvaginal ultrasound can help detect ovarian cysts (endometriomas) and adhesions.
◦ While ultrasound may not detect small lesions, it is often the first step in evaluation.
3. Magnetic Resonance Imaging (MRI):
◦ Provides detailed images of pelvic structures, useful for identifying deep infiltrating endometriosis.
4. Laparoscopy (Gold Standard):
◦ A minimally invasive surgical procedure that allows direct visualization of endometrial tissue.
◦ Laparoscopy not only confirms the diagnosis but may also allow the removal of endometriotic lesions.
Treatment Options Based on Stage
The treatment for endometriosis varies depending on the stage, severity of symptoms, and reproductive goals. A combination of medication, surgery, and assisted reproductive techniques (ART) may be recommended to manage pain and improve fertility outcomes.
Stage 1: Minimal
• Treatment Approach:
◦ Pain Management: Over-the-counter pain relievers, such as anti-inflammatory medications, can help manage mild discomfort.
◦ Hormonal Therapy: Birth control pills, progestins, or GnRH agonists may be prescribed to reduce inflammation and slow tissue growth.
• Fertility Impact: Minimal impact on fertility, but in cases of unexplained infertility, assisted reproductive technologies such as intrauterine insemination (IUI) may be considered.
Stage 2: Mild
• Treatment Approach:
◦ Hormonal Therapy: Hormonal treatments to suppress endometrial tissue growth and alleviate symptoms.
◦ Laparoscopic Surgery: Minimally invasive surgery may be performed to remove superficial implants and adhesions, improving the chances of conception.
• Fertility Impact: While mild endometriosis may not always affect fertility, laparoscopic surgery can improve reproductive outcomes, especially in cases where scarring is present.
Stage 3: Moderate
• Treatment Approach:
◦ Laparoscopic Surgery: Surgery is often recommended to remove deep implants, cysts (endometriomas), and adhesions. This helps restore pelvic anatomy and improve fertility.
◦ Hormonal Suppression Post-Surgery: Hormonal therapy may be used after surgery to prevent the recurrence of endometrial tissue.
• Fertility Impact: Moderate endometriosis can significantly impact fertility. If conception is not achieved naturally after surgery, assisted reproductive techniques like in vitro fertilization (IVF) may be suggested.
Stage 4: Severe
• Treatment Approach:
◦ Laparoscopic or Advanced Surgery: Extensive surgery may be required to remove large endometriomas, deep implants, and adhesions affecting pelvic organs.
◦ IVF or ART: Due to extensive damage and compromised pelvic anatomy, IVF is often the most effective option for achieving pregnancy in severe cases.
◦ Pain Management: For women not seeking pregnancy, hormonal therapies and pain management strategies are used to control symptoms.
• Fertility Impact: Severe endometriosis greatly reduces the chances of natural conception. IVF can bypass the fallopian tubes and optimize fertilization and implantation.
Conclusion: Importance of Early Detection
Why Early Detection Matters
Timely diagnosis and management of endometriosis can significantly improve a woman’s quality of life and reproductive outcomes. Early detection helps:
• Prevent Progression: Minimizing tissue growth and preventing complications.
• Manage Pain Effectively: Reducing the need for invasive treatments in later stages.
• Improve Fertility Prospects: Enhancing the chances of conception through less invasive approaches.
Signs to Watch For
Women experiencing chronic pelvic pain, painful periods, pain during intercourse, or unexplained infertility should seek medical evaluation. A thorough assessment, including ultrasound and laparoscopy if necessary, can help confirm the diagnosis and determine the appropriate treatment plan.
Final Note
For women diagnosed with endometriosis, individualized treatment plans that address both pain management and fertility goals are essential. Consulting a fertility specialist early on can help optimize outcomes, whether through medical management, minimally invasive surgery, or assisted reproductive techniques. For those seeking female infertility treatment in Vizag, timely intervention can significantly enhance the chances of conception and improve overall reproductive health.
