What is Endometrial Thickness in IVF?
Endometrial thickness refers to the measurement of the uterine lining, which plays a critical role in the success of IVF treatment. It is evaluated through transvaginal ultrasound during the fertility treatment cycle. A well-prepared endometrium is crucial for embryo implantation and the establishment of a pregnancy. Factors like hormonal balance, uterine health, and blood flow contribute to optimal endometrial growth. For those seeking effective solutions, consulting specialists for female infertility treatment in Vizag can help address challenges and improve the chances of successful pregnancy.
What is the Optimal Range for Endometrial Thickness?
In IVF, the ideal endometrial thickness is typically between 7mm to 14mm during the implantation window. A lining thinner than 7mm may decrease the chances of implantation, while an excessively thick lining may also impact success rates. A trilaminar (three-layered) appearance of the endometrium on ultrasound is considered a positive indicator of uterine receptivity.
Monitoring and optimizing endometrial thickness are essential steps in IVF, ensuring the uterus is ready to support a healthy pregnancy.
What is the Optimal Endometrial Thickness in IVF?
When it comes to In Vitro Fertilization (IVF), the endometrial thickness plays a vital role in determining the success of the procedure. A well-prepared uterine lining ensures that the embryo has a conducive environment to implant and develop. Let’s dive into the significance of endometrial thickness and the factors that influence it.
Role of Endometrial Thickness in IVF Success
1. Foundation for Implantation The endometrium, or uterine lining, is the tissue that lines the inside of the uterus. During the IVF process, achieving an optimal endometrial thickness is critical. Research indicates that a thickness of 7-14 mm during the time of embryo transfer is ideal for successful implantation.
2. Triple-Layered Pattern Apart from thickness, the appearance of the endometrium on an ultrasound also matters. A trilaminar or “triple-striped” pattern is associated with higher implantation rates, indicating a receptive lining.
3. Hormonal Synchronization Estrogen and progesterone play key roles in preparing the endometrium. Estrogen thickens the lining, while progesterone supports its transformation into a receptive state. Imbalances in these hormones can result in suboptimal thickness or poor quality of the endometrium.
4. Improved Blood Flow Adequate blood flow to the uterine lining ensures proper nutrient and oxygen delivery, essential for embryo implantation and growth. Thin endometrium often correlates with poor vascularization, reducing IVF success rates.
5. Indicator of Uterine Health The endometrial thickness can also act as a marker for uterine health. A persistently thin or overly thick lining may indicate underlying issues like scarring (Asherman’s syndrome) or polyps, which can hinder successful implantation.
Factors Affecting Endometrial Thickness
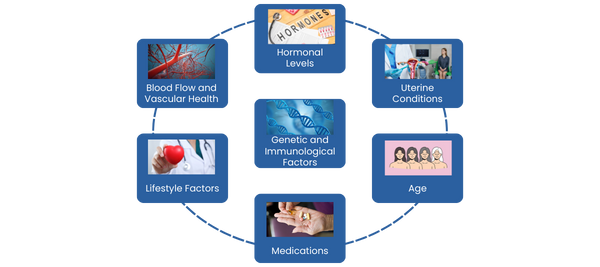
1. Hormonal Levels
◦ Estrogen Levels: Low estrogen levels can result in a thin endometrium, making it less receptive to embryo implantation.
◦ Progesterone Levels: Insufficient progesterone can prevent the lining from maturing adequately, impacting its ability to support an embryo.
2. Uterine Conditions
◦ Fibroids: Uterine fibroids can distort the uterine cavity, affecting the endometrial lining’s uniformity and thickness.
◦ Polyps: These growths can interfere with the even distribution of the uterine lining, making it less receptive.
◦ Scarring: Conditions like Asherman’s syndrome can result in a thin or irregular endometrium.
3. Age With age, the quality of the uterine lining may decline, affecting its receptivity. Women over 35 may experience a thinner or less responsive endometrium.
4. Medications Certain medications, such as clomiphene citrate, can negatively affect endometrial thickness. However, medications like estrogen supplements and sildenafil (under medical supervision) are often prescribed to improve thickness.
5. Lifestyle Factors
◦ Nutrition: A diet rich in vitamins like vitamin E, L-arginine, and omega-3 fatty acids supports uterine blood flow and endometrial health.
◦ Stress: High stress levels can alter hormonal balance, indirectly affecting endometrial thickness.
◦ Exercise: While moderate exercise promotes blood circulation, excessive or intense physical activity can have the opposite effect.
Related- How to Prepare Yourself Physically and Mentally for IVF Treatment
6. Blood Flow and Vascular Health Conditions like diabetes or high blood pressure can impair blood flow to the uterus, leading to a thinner endometrial lining.
7. Genetic and Immunological Factors Some women may have inherent genetic or immunological issues that impact their endometrial receptivity, making IVF success more challenging.
Improving Endometrial Thickness: Possible Solutions
1. Lifestyle Modifications
◦ Balanced Diet: Incorporate foods rich in antioxidants, omega-3 fatty acids, and iron to improve uterine health. Leafy greens, nuts, seeds, and fatty fish like salmon are excellent choices.
◦ Regular Exercise: Moderate physical activity improves blood flow to the uterus, promoting a thicker and healthier endometrium.
2. Medical Interventions
◦ Estrogen Therapy: Estrogen supplements, often prescribed during IVF cycles, help build and maintain the endometrial lining.
◦ Low-Dose Aspirin: Sometimes used to enhance blood flow to the uterine lining, aiding in endometrial growth.
◦ Platelet-Rich Plasma (PRP) Therapy: An emerging technique, PRP injections into the uterus may help improve endometrial thickness in challenging cases.
3. Natural Remedies
◦ Acupuncture: Promotes uterine blood flow and hormonal balance, supporting endometrial development.
◦ Herbal Supplements: Some herbal remedies, like those containing L-arginine and vitamin E, have shown promise in improving uterine lining. Always consult your doctor before trying supplements.
4. Addressing Underlying Conditions
◦ Conditions like polyps, fibroids, or endometriosis may hinder endometrial growth. Treating these issues can significantly improve implantation outcomes.
5. Adequate Hydration
Staying hydrated improves blood circulation throughout the body, including the uterus, aiding in optimal endometrial health.
6. Hormonal Balance
Maintaining proper hormonal levels through medications or natural methods is essential for a receptive endometrium.
Conclusion
Maintaining an optimal endometrial thickness is vital for successful IVF outcomes. Lifestyle changes, medical interventions, and addressing any underlying health conditions can significantly improve the chances of embryo implantation.
For anyone facing challenges with endometrial health, consulting the best IVF doctor in Visakhapatnam is crucial. Personalized care and treatment can make a significant difference in overcoming these hurdles and ensuring a successful pregnancy.
